HTML
-
Respiratory tract infections (RTIs) including influenza are important health hazards among travellers with the incidence of influenza in returning febrile travellers from subtropical and tropical regions being between 5 and 15% (Askling H H, et al., 2010; Belderok S M, et al., 2013, Davis X M, et al., 2013). GeoSentinel data for the 2009 pandemic influenza showed that detection of travel-related cases could be a reliable indicator of sustained influenza transmission within the exposure country and may aid planning for control measures (Davis X M, et al., 2013). Mass gathering events such as the Hajj pilgrimage, the Olympic Games or the Football World Cup are known to amplify the risk of transmission of respiratory viruses including escalating pandemic influenza (Blyth C C, et al., 2010; Haworth E, et al., 2013; Zepeda-Lopez H M, et al., 2010). For instance, it is postulated that a mass event that took place in Iztapalapa, Mexico sparked the rapid global dissemination of H1N1/09 influenza (Zepeda-Lopez H M, et al., 2010).
During Hajj, up to 3 million pilgrims assemble in Mecca city before moving in a body to Mina (a small valley at the outskirts of Mecca), where they live in tents shared by, depending on size, between 30 and 150 persons. The interplay of multitude of factors including severe crowding, limited facilities and time for personal hygiene, and particulate and microbiological air pollution at Hajj increases the risk of acquisition of respiratory viruses by up to 8 fold (Benkouiten S, et al., 2013; Hameed A A, et al., 2013; Haworth E, et al., 2013; Rashid H, et al., 2008). The emergence of the Middle East respiratory syndrome coronavirus (MERS-CoV) in the Gulf region with its epicentre in Saudi Arabia has raised major concern over the possibility of home-bound pilgrims' spreading of MERS-CoV globally (Al-Tawfiq J A, et al., 2014; Rashid H, et al., 2014). Limited virological and syndromic surveillance data during the Hajj 2012 did not show Hajj-associated transmission of MERSCoV (Gautret P, et al., 2014, Rashid H, et al., 2014), but the virus was detected in pilgrims who visited Mecca and Medina on Umrah pilgrimage 2012 and 2013 (Devi J P, et al., 2014; Health Protection Agency (HPA) UK Novel Coronavirus Investigation team, 2013).
Two studies attempted to assess the prevalence of MERS-CoV and influenza among pilgrims during the Hajj 2013 (Memish Z A, et al., 2014, Benkouiten S, et al., 2014). These studies provided timely and valuable data, but had some methodological limitations: one provided airport-based surveillance data and therefore did not reflect the true Hajj epidemiology (Memish Z A, et al., 2014), while the other, although conducted at the Hajj site and studied an array of bacterial and viral pathogens, involved only one travel group of pilgrims from Marseille and therefore may not be generalisable to other pilgrims (Benkouiten S, et al., 2014). In the current report we present the data on the attack rate of common respiratory viruses among symptomatic pilgrims from Saudi Arabia, Australia and Qatar who participated in a large trial assessing the efficacy of facemasks against respiratory infections including MERS-CoV during the Hajj 2013.
-
The protocol of this study is published in detail elsewhere (Wang M, et al., 2014). Breifly, pilgrims from Saudi Arabia, Australia and Qatar were recruited in a large-scale cluster-randomised controlled trial to assess the efficacy of facemasks in the prevention of respiratory viruses including influenza and MERS-CoV among Hajj pilgrims. This report analyses data from symptomatic pilgrims only.
At the Hajj 2103, conveniently placed individual tents accommodating Hajj pilgrims from Saudi Arabia, Australia or Qatar were randomly assigned to 'supervised use of facemasks' versus 'standard infection control measures' recommended by Saudi Ministry of Health (MoH). Every member of each participating tent was eligible to participate in the study. During the morning and afternoon of the first day of Hajj (13th October, 2013), research team members consisting of physicians and trained medical students explained the study to the pilgrims in each tent, and invited those aged 18 years or older to participate in the study voluntarily.
Participants who consented were asked to complete a baseline questionnaire on 13th October, 2013 that included contact details, relevant demographics, vaccination history and clinical information including current respiratory symptoms with duration and pre-existing medical conditions. Participants were provided with diaries that had a unique barcode number for identification. The pilgrims recorded on the dairies the severity and outcome of new or continuing influenza-like illness (ILI). Diaries were collected on the conclusion of Hajj on 16th October 2013.
Pilgrims aged ≥ 65 years, and/or with pre-existing medical illnesses such as chronic lung, heart, kidney, liver, neuromuscular, metabolic or immunocompromising conditions were defined as 'at risk' individuals since they were at higher risk of developing severe complications from influenza infections (Memish Z A, et al. 2014).
-
Each day, the research team members visited the tents and actively searched for pilgrims who had developed ILI, defined as subjective (or proven) fever and at least one respiratory symptom such as cough, sore throat and rhinorrhoea. Nasopharyngeal (NP) swabs (or a throat swab if NP swab was not possible) were taken from pilgrims with an ILI by a trained team member using Copan Nylon® Flocked swabs placed in Universal Transport Medium (UTMTM [Copan Italia, Brescia, Italy]). Swabs were frozen at -80 ℃ within the same day of collection and stored at the same temperature until tested at Westmead Hospital, New South Wales, Australia. The shipping process took about 2 months because the swabs could not be moved until after the Jeddah airport's cold storage facilities had been repaired and certified effective.
Nucleic acid extraction was performed using the Qiagen bioROBOT EZ instrument (Qiagen, Valencia, CA), and amplification carried out using the Roche LC 480 (Roche Diagnostics GmbH, Mannheim, Germany) real-time instrument. Respiratory viruses were detected using a real-time, multiplex RT-PCR assay targeting human coronaviruses (OC43, 229E and NL63), influenza A, influenza B, respiratory syncytial virus, parainfluenza viruses 1–3, human metapneumovirus, rhinovirus, enterovirus and adenoviruses as described in detail elsewhere (Ratnamohan V M, et al., 2014; Gaunt E R, et al., 2010). A MERS-CoV assay targeting regions upstream of the E gene (upE) was also performed as described previously (Corman V M, et al., 2012).
This study was approved by the Hunter New England Human Research Ethics, Australia (Ref: 13/07/17/3/04), Hamad Medical Corporation/Weill Cornell Medical College in Qatar Joint Institutional Review Board, Qatar (Ref: 13-00039) and by the Saudi Ministry of Health.
Study protocol
Specimen collection and testing
-
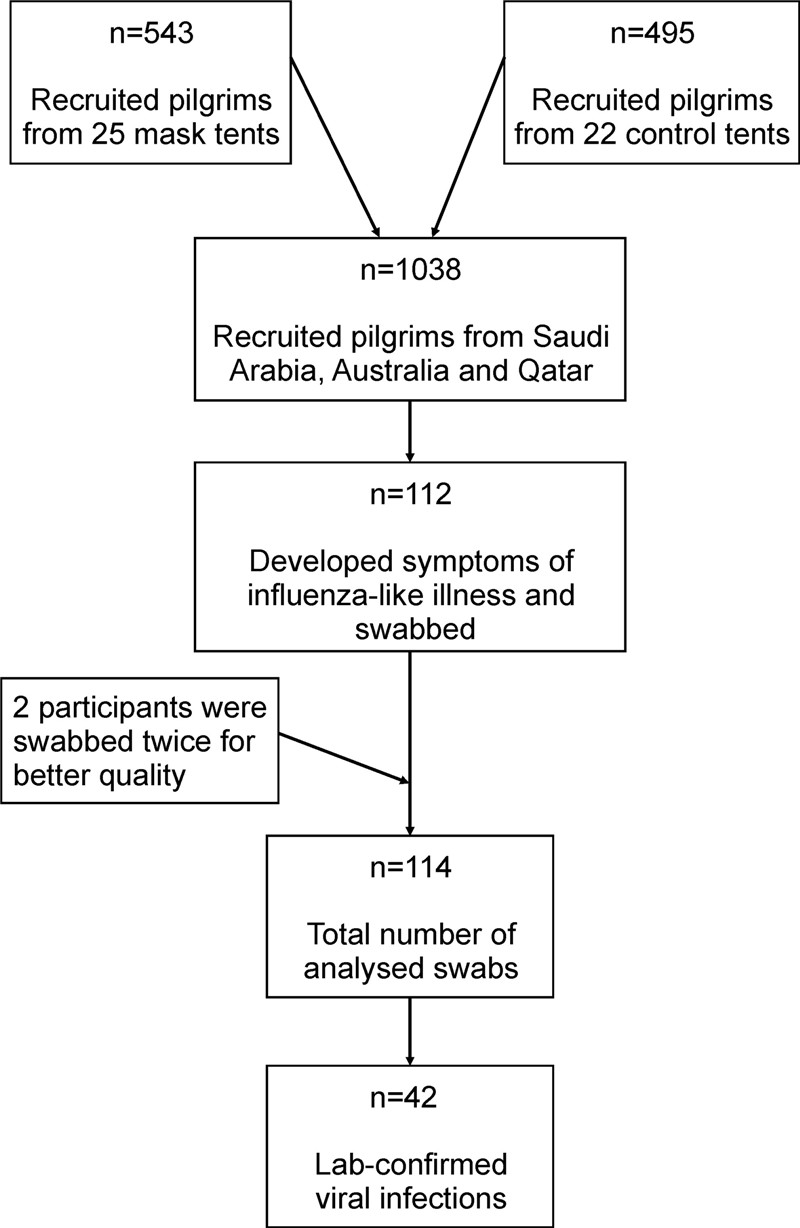
A total of 1038 pilgrims were recruited from 47 tents and followed during the peak period of Hajj in 2013 (Figure 1). Of the recruited pilgrims, 443 (43%) were male, 923 (89%) were from Saudi Arabia, 90 (9%) from Australia and 25 (2%) from Qatar.
The prevalence of ILI among the recruited pilgrims was 11% (112/1038). NP swabs were collected from all symptomatic pilgrims; initially throat swabs were collected from two participants but from them too eventually NP swabs were collected (Figure 1). They were aged between 18 and 75 (mean 35) years. The participants' demographic characteristics are described in Table 1 according to their country of origin.
Pilgrims' country of origin Saudi Arabia n (%) Australia n (%) Qatar n (%) Number of symptomatic participants 92 15 5 Median age in years (range) 34 (18–62) 40 (25–61) 56 (31–75) Gender 38 (41%) male 6 (40%) male 5 (100%) male 'At risk'* 17 (19%) 3 (20%) 2 (40%) Received influenza vaccine in 2013 18 (20%) 13 (87%) 4 (80%) Visit medical centres during Hajj 9 (10%) 2 (13%) 0 Lab-confirmed infection 33 (36%) 7 (47%) 2 (40%) Viruses Rhinovirus 21 (22.8%) 6 (40%) 1 (20%) Influenza 5 (5.4%) -- -- Parainfluenza 3 2 (2.2%) -- -- Adenovirus 2 (2.2%) -- -- Coronavirus (OC43/229E) 2 (2.2%) -- -- Parainfluenza 1 -- -- 1 (20%) Rhino + coronavirus -- 1 (6.7%) -- Rhino + adenovirus 1 (1.1%) -- -- *Pilgrims aged ≥ 65 years, and/or with pre-existing medical illnesses such as chronic lung, heart, kidney, liver, neuromuscular, metabolic or immunocompromising conditions were considered 'at risk'. Table 1. Demography and virology of 112 Hajj pilgrims with respiratory symptoms in 2013 by country of origin
Twenty two (20%) of those reporting ILI were considered 'at risk' of acquiring respiratory infections due to their age ≥ 65 years (2 [9%]), or coexisting of chronic medical conditions such as chronic respiratory diseases (15 [68%]), diabetes (9 [41%]), cardiac diseases (1 [4%]) or renal disorders (1 [4%]). Only 35 (31%) of these symptomatic pilgrims reported receiving influenza vaccine before Hajj. The uptake of influenza vaccine among Australian, Qatari and Saudi pilgrims was 87%, 80% and 20% respectively.
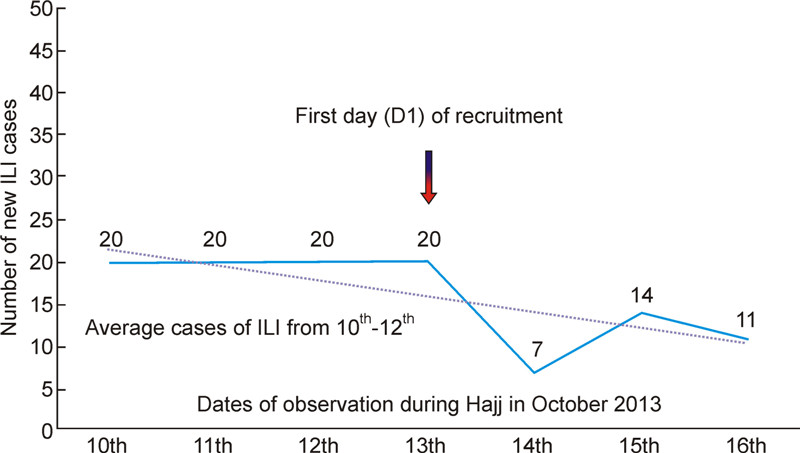
Sixty (54%) pilgrims fulfilled ILI definition at the time of recruitment. On D1-Sunday 13th of October 2013–20 (18%) fresh new cases of ILI were reported; 7 (6%) new cases on D2, Monday the 14th; 14 (12%) on D3, Tuesday the 15th, and 11 (10%) on D4, Wednesday the 16th (Figure 2). The most common respiratory symptom was sore throat 66 (59%), followed by cough 45 (40%) and runny nose 38 (34%). Of the 112 symptomatic pilgrims, only 11 (10%) visited clinics or health care centres in Mecca for ILI or RTI symptoms. Forty two (38%) pilgrims had laboratory-confirmed viral infections: 28 (25%) rhinovirus, 5 (4%) influenza A (4 H3N1 and 1 H1N1/09), 2 (2%) adenovirus, 2 (2%) human coronavirus OC43/229E, 2 (2%) parainfluenza virus 3, 1 (1%) parainfluenza virus 1, and 2 (2%) dual infections (rhinovirus/adenovirus and rhinovirus/human coronavirus OC43/229E) (Table 1). The rate of influenza in vaccinated pilgrims was similar to that in unvaccinated pilgrims (5.2% [4/77] versus 2.9% [1/35]), P = 0.58). MERS-CoV was not detected in any sample.
-
This study showed that the point-prevalence of ILI among pilgrims from Saudi Arabia, Australia and Qatar who volunteered to participate in this study during the Hajj 2013 was 11%, and that 38% (42/112) of symptomatic pilgrims had laboratory-confirmed viral infections which is comparable to a virus detection rate of 38.6% among French pilgrims during the Hajj 2012 (Benkouiten S, et al., 2013). This rate of ILI was lower than that was seen in French pilgrims (47%) during the same year, however in the latter, 91% subjects had at least one respiratory symptom (Benkouiten S, et al., 2014); an unpublished report involving Malaysian pilgrims showed that 86% suffered from ILI during the Hajj 2013, with prevalence varying according to the geographic locations within Mecca (Dr Habsah Hasan, Kelantan, Malaysia, personal communication). A decline in ILI rates over the next few days of stay in Mina is interesting and unexpected (Figure 2), but its significance is unexplained at this stage. It is possibly because of the effect of facemask use in many pilgrims, but these data are insufficient to support or refute this notion.
Studies conducted over the past few years have shown that the prevalence of ILI among Hajj pilgrims varies by country of origin and by year. For instance, in 2012, approximately 9% of Australian pilgrims compared to 41% of French pilgrims had respiratory symptoms, which was consistent with the findings for 2013 Hajj (Gautret P, et al., 2014; Rashid H, et al., 2013). However, in a pilot study conducted by our team we observed that 44% of Australian pilgrims had ILI during the Hajj 2011 (Barasheed O, et al., 2014), however only 8% of French Hajj pilgrims reported having ILI in 2009 (Gautret P, et al., 2011). During the Hajj 2007, 40% Malaysian pilgrims developed ILI (Deris Z Z, et al. 2010). Such disparity can be explained by factors such as differences in age and prevalence of underlying chronic diseases, as well as seasonal and geographic variations in respiratory virus circulation. The average age among our participants was 35 years and only 20% had an underlying chronic disease. This contrasts to the situation seen in French pilgrims whose mean age was 62 years and where 53% had chronic underlying medical conditions (Benkouiten S, et al., 2014). Also, it is noteworthy that the definition of ILI deferred across the studies. No MERS-CoV was detected in any of the pilgrims in this study; this corroborates the findings of both the French study and Saudi airport-based surveillance for MERS-CoV, neither of which identified this virus among pilgrims who attended Hajj 2013 (Memish Z A, et al., 2014; Benkouiten S, et al., 2014).
Despite this absence of laboratory confirmed MERSCoV among Hajj pilgrims, a spike in MERS cases occurred in April 2014 in Saudi Arabia, importantly in the port city of Jeddah through which most pilgrims enter and leave Mecca (Alghamdi I G, et al., 2014). In addition, the Malaysian Ministry of Health reported a fatal case of laboratory-confirmed MERS-CoV infection in a 54 year old man returning from Umrah pilgrimage at the end of March 2014; the patient visited a camel farm and drank camel milk (Devi J P, et al., 2014). Another laboratory-confirmed case of MERS-CoV was reported in a 69 year old Greek man who returned from Jeddah; this individual did not report any contact with camels, but regularly visited his wife who was hospitalised in Jeddah for enteric fever (Tsiodras S, et al., 2014). Similarly, the first two confirmed cases of MERS-CoV infection in North America was reported in US healthcare workers, aged ≥ 60 and ≥ 40 years respectively, who lived and worked in hospitals in Saudi Arabia where patients with MERS had received care (Bialek S R, et al., 2014). These updates indicate that enhanced surveillance is urgently required to tease out the modality of transmission, and explore effective preventive measures and potential therapeutic interventions.
The commonest cause of ILI in our study was rhinovirus which was detected in 25% of symptomatic pilgrims. Similarly, rhinovirus was the most common cause of ILI among British pilgrims in 2006 (14%), international pilgrims (arriving from the Middle East, Asia and Africa) in 2009 (13%) and French pilgrims in 2012 (27%) (Benkouiten S, et al., 2013; Memish Z A, et al., 2012; Rashid H, et al., 2008). In addition, rhinovirus infections were reported among Iranian pilgrims in 2006 and subsequently among non-Hajj travellers during the onset of the pandemic A (H1N1) influenza in 2009 (Alborzi A, et al., 2009; Jaureguiberry S, et al., 2012). Although rhinovirus infection is usually relatively mild, it can lead to hospitalisation of the patients with chronic medical condition (Walker E, et al., 2014).
The attack rate of influenza virus in our symptomatic pilgrims was only 4% (5/112) during the Hajj 2013, whereas the prevalence of influenza virus among the French pilgrims in the same year was 7.8% (Benkouiten S, et al., 2014). Observing the global influenza activity at the time of Hajj, experts opined that pilgrims from tropical Africa might have introduced the virus at the Hajj 2013 and thus facilitated its spread among European pilgrims (Raoult D, et al., 2014). Only 3.2% of returning French Hajj pilgrims had influenza in the year 2012 (Benkouiten et al., 2013). During the 2009 influenza pandemic, the prevalence of influenza virus infection (including H1N1/09) among international Hajj pilgrims was 0.2% (Memish Z A, et al., 2012). In 2006, the influenza attack rate was reported to be 10% in Saudi Arabian, British and Iranian Hajj pilgrims (Alborzi A, et al., 2009; Rashid H, et al., 2008), while in 2005, the attack rate among UK pilgrims was 14% (Rashid H, et al., 2008). These differences may be due to varying methodology, sample size, influenza vaccine uptake or seasonal variations of influenza in pilgrims' countries of origin or change of season of the Hajj that happens with Hajj moving 10-12 days forward in the Gregorian calendar.
The strength of this study is that these data originate from a large sample size (1038), and the pilgrims were closely followed for the 4 peak days of Hajj. Furthermore, the timing, site of recruitment and follow-up of this study was conducted at the main Hajj spot (Mina) during the most intense Hajj activities, so that it presents more representative Hajj epidemiology. In our study throat swabs were obtained from only two participants, but from them too ultimately NP swabs were obtained, a recent study has confirmed that nasal swabs are superior in detecting common respiratory viruses among Hajj pilgrims (Benkouiten S, et al., 2014). However, nasal or nasopharyngeal swabs have been shown to be poor in detecting MERS-CoV in people with pneumonia; lower respiratory tract samples such as sputum or preferably bronchoalveolar lavage samples produce better yields (Memish Z A, et al., 2014). Also, it should be noted that these data derive from symptomatic patients recruited in a randomised controlled trial, asymptomatic individuals were not swabbed, and the effect of facemask has not been explored. The trial continues (Wang M, et al., 2014), and the full results will be published once the required number of participants is obtained.
In summary, MERS-CoV was not detected in a target population of 1038 pilgrims from Saudi Arabia, Australia and Qatar during the peak period of Hajj in 2013. Amongst 112 pilgrims with respiratory symptoms, rhinoviruses were the most common respiratory viruses identified, and several other respiratory viruses including influenza, adenovirus, coronaviruses and parainfluenza viruses were also detected. Infection control measures to minimise the risk of transmission of respiratory viruses and relevant vaccination, particularly for influenza, should continue as methods to prevent transmission of respiratory viruses at Hajj and other mass gatherings.
-
This report was made possible by a National Priorities Research Program grant (NPRP 6-1505-3-358) from the Qatar National Research Fund (a member of Qatar Foundation). ECH is supported by an NHMRC Australia Fellowship.The authors acknowledge the help and support of: the Royal Embassy of Saudi Arabia, Canberra; Saudi Arabian Cultural Mission, Canberra; Ministry of Higher Education, Riyadh; Ministry of Health, Riyadh; Ministry of Hajj (Deputy Minister's Office), Mecca; the Custodian of the two Holy Mosques Institute for Hajj and Umrah Research (Dr. Abdulaziz Seroji and Dr. Turki Habeebullah), Mecca.
-
Professor Robert Booy and Dr Leon Heron have received funding from Baxter, CSL, GSK, Merck, Novartis, Pfizer, Roche, Romark and SanofiPasteur for the conduct of sponsored research, travel to present at conferences or consultancy work; all funding received is directed to research accounts at The Children's Hospital at Westmead. The other authors have declared no conflict of interest in relation to this work.
-
OB executed the trial, analysed data and prepared the first draft of the manuscript; HR is the guarantor of the study, and oversaw implementation of the study, contributed to data analysis and manuscript preparation; MAF, MT, MA, HB, NK and JS participated in data collected and contributed to the manuscript; LH supervised preparation of the research protocol and research tools; JK and JT were responsible for conducting molecular diagnostic tests; HEB contributed to data interpretation; ZAM contributed to study design; EH contributed to the study design and supervised data analysis and interpretation; ECH and DED contributed to the design and interpreted molecular diagnostic tests; AA contributed to the collection, analysis and interpretation of data; RB supervised data interpretation and overseen manuscript revision; Hajj Research Team participated in data collection and sorting logistics.
**Hajj Research Team:
[Ibtihal Malawi, Ebtehal Matar, Abrar Tawakoul, Abrar ALnami, Atheer Alshareif, Israa Kalantan, Asal Arbaeen, Eatimad Alalawi, Afnan AlGhamdi, Amani Koshak, Ameerah Alkhaldi, Enasm Al-Nami, Anwar Howsawi, Bashaier Fairaq, Bushra Maghrabi, Tafaol Murad, Hanan Alzahrani, Kholood Almehmadi, Doaa Milibari, Rehab Hafiz, Rawdhah Kalantan, Shahad Al-Ansari, Aeshah Rajab, Anood Alfahmy, Ghaida Ali, Fatimah Abu naji, Lujin Hassan, Lulwah Althumali, Layla Farhat, Najlaa Baddour, Hibh Alandanusi, Waad Alqurashi, Sumayyah Fallata, Azhar Alharbi, Joud Bahakeem, Abrar Alshareef, Badr Rawa, Daniah Alnemari, Mawadah Hariri, Samah Alhadramy, Ahmed Alghamdi, Ahmed Muqadimi, Ahmad Bimah, Osama Alamri, Jehad Qutub, Abdulrahman Al-Ghamdi, Abdurrahman Mirza, Abdulghafur Alandijani, Omar Qoqandi, Faisal Mandourah, Muhammad Alghamdi, Mohammed Mahboob, Mohannad Alsulami, Moayyd Hinnawi, Naif Hawsawi, Mousab Alsudais, Nawaf Dhabab, Ahmed Balamash, Mohammed Bawazir, Raif Nassir, Mohammed AlAsmari, Faisal Alzahrani, Abdulrahman Alomari and Ahmad Makeen]












 DownLoad:
DownLoad: