-
Several recent studies in Virologica Sinica and other journals have highlighted the enormous international challenge of emerging arboviral diseases, such as Zika virus disease, dengue, and chikungunya (Islam et al., 2015; Maurice et al., 2015; Dai et al., 2016; Deng et al., 2016; Song et al., 2016; Wang Z et al., 2016; Xu et al., 2016; Zhang et al., 2016; Zhou et al., 2016). Rift Valley fever (RVF) is a mosquito-borne disease caused by the Rift Valley fever virus (RVFV), which causes high levels of mortality and morbidity in domesticated animals and mild to serious disease in humans. Since the virus was first described in Kenya in 1931 (Daubney et al., 1931), no extensive human outbreaks of this disease were reported until 1951, when approximately 20, 000 individuals were infected in South Africa (Mundel and Gear, 1951). Subsequently, there have been several RVF outbreaks with significant impact on human health in eastern Africa and the Arabian Peninsula (Meegan, 1979; CDC, 1998; Shoemaker et al., 2002; Woods et al., 2002) (http://www.who.int/csr/don/2007_05_09/en/). At present, RVFV is present or endemic in almost all African nations, as well as Saudi Arabia and Yemen in the Arabian Peninsula (Figure 1), and has the potential to expand to other regions.
RVFV can be transmitted by many mosquito species (mainly from the genera Aedes and Culex), as well as flies and ticks (Davies and Highton, 1980), and outbreaks of RVF are closely linked to heavy rainfall or flooding (Sindato et al., 2011). In addition, wildlife and livestock may play an important role in outbreaks in humans. Human cases are primarily caused by bites from infected mosquitoes or by direct contact with tissues or fluids from infected animals (Anyangu et al., 2010; Baba et al., 2016); In addition, vertical transmission has also been reported in mosquito vectors, ruminants, and humans (Arishi et al., 2006; Adam and Karsany, 2008). In humans, the disease can present with fever, headache, arthralgia and muscle pain, acute hepatitis, or hemorrhagic and neurological manifestations, and the fatality rate can reach 50% in patients with hemorrhagic complications (Swanepoel et al., 1979; Madani et al., 2003). Although there are three approved veterinary vaccines, no vaccines are available for human use (http://www.oie.int/manual-of-diagnostic-tests-and-vaccines-for-terrestrial-animals/).
HTML
-
On July 21, 2016, a 45-year-old male who had been working in Luanda, Angola, returned to China (Figure 1). He had been suffering symptoms of headache, fever, arthralgia and muscle pain since July 14, and had received treatment in a local hospital in Angola. However, the symptoms persisted, and he arrived in Beijing Capital International Airport in serious condition (http://www.who.int/csr/don/02-august-2016-rift-valley-fever-china/en/). Two days later, the National Health and Family Planning Commission of the People's Republic of China reported this as the first imported case of Rift Valley fever in China (http://www.aqsiq.gov.cn/xxgk_13386/tsxx/yqts/201608/t20160803_471831.htm).
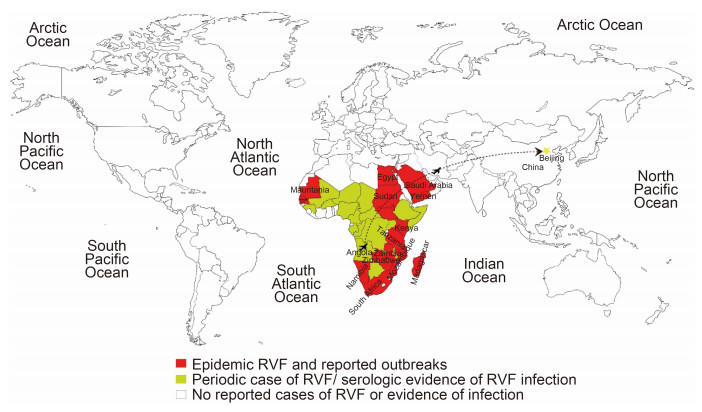
Figure 1. Map of the global distribution of Rift Valley fever virus (RVFV), referenced from the map published by the Centers for Disease Control and Prevention of USA (http://www.cdc.gov/vhf/rvf/outbreaks/distribution-map.html). Countries in which RVF is endemic or has caused significant outbreaks are shown in red, countries with periodic cases of RVF and/or serological evidence of infection are shown in yellow, countries in white have no reported cases of RVF or evidence of infection. The black dotted line shows the case import from Angola to China.
-
The RVF outbreak that occurred in Saudi Arabia and Yemen in 2000 resulted in 2171 infections and 245 deaths (Shoemaker et al., 2002), and this outbreak is reported to have been caused by the same strain of the RVF virus that caused the outbreak in Kenya in 1997–1998 (Shoemaker et al., 2002). The outbreak in Saudi Arabia and Yemen in 2000 was caused by infected animals imported from Kenya (Baba et al., 2016). Confronted with this imported case, the government in China has implemented surveillance, monitoring, and other measures to prevent the spread of RVF in China (http://www.nhfpc.gov.cn/yjb/s3578/201607/e1fc91f93d034bd0b952b8745356bd65.shtml). However, because conditions for the spread of RVF are currently present in China, there is a risk that RVF may spread from this imported case. Firstly, mosquitoes, the RVF vector, are very active in summer, and Aedes mosquitoes are widely distributed in China, especially Southern China. Secondly, there have been several rounds of heavy rainfall since June, and many provinces have experienced flooding. Based on the lessons learned during the outbreaks in Saudi Arabia and Yemen, and given these conditions, there is a high risk that the imported case may spread or even cause an outbreak, if proper measures to prevent and control RVF are not implemented.
Early detection of suspected cases is the key to ensure that timely control measures are implemented to prevent the spread and outbreak of emerging or re-emerging infectious diseases, such as Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), and Ebola, as well as RVF (Wong et al., 2015). However, cases of human infection with RVFV are generally asymptomatic, and most result in no more than a short febrile illness (Madani et al., 2003); some animals may experience an inapparent infection (Mansfield et al., 2015). This is another challenge to detection of suspected cases.
-
Because it is a vector-borne disease, mosquitoes (especially Aedes and Culex) play an important role in the spread and outbreak of RVF; thus, eliminating the vector and preventing mosquito bites are the most effective means to control the spread of RVF. Enhanced surveillance and monitoring of the numbers and infection level of the vector are also important. In addition, infection of livestock is a risk factor, because humans can be infected by direct contact with infected animals (Anyangu et al., 2010) and mosquitoes can spread RVFV via infected animals. It is therefore advisable to suspend trading of livestock with countries experiencing an RVF epidemic and to implement a strong quarantine. Meanwhile, the effectiveness of strengthening collaboration and coordination across sectors, such as government, the Centers for Disease Control and Prevention, researchers, and hospitals, to make prevention and control measures more efficient, was demonstrated when the MERS case was imported in China (Su et al., 2015; Su et al., 2016b) and during the RVF outbreak in Saudi Arabia (Himeidan et al., 2014). Development of an effective vaccine for prevention of RVF is urgent for both humans and animals.
China has a large population, and its climate and the wide distribution of the mosquito vectors in south China are high risk factors for RVF outbreak. More importantly, once RVFV is introduced into permissive ecologies, it can become endemic, with the potential to spread into other non-endemic regions (Murithi et al., 2011). If there is an RVF outbreak in China, the disease may spread quickly to Southeast Asia and to other countries in Asia. Combined with the import of the Zika and yellow fever viruses this year (Su et al., 2016a; Wang L. et al., 2016), importation of arboviral pathogens poses a huge challenge for China. Therefore, all necessary measures should be taken to prevent and control RVF import and spread in China in the future.
-
This project was supported in part by the National Natural Science Foundation of China (Grant No. 31402224 and 31272564), the Public Welfare Special Funds for Agriculture Scientific Research (Grant No.201203039), and the Modern Agro-Industry Technology Research System (CARS-36). The authors declare that they have no conflict of interest. This article does not contain any studies with human or animal subjects performed by any of the authors.













 DownLoad:
DownLoad: