-
Alzheimer's disease (AD), also known as Alzheimer's, is a chronic neurodegenerative disorder with hallmark amyloid plaques in brain tissue. The diseases commences slowly and worsens over time (Sjogren et al. 1952). Although it has been investigated for over six decades, the cause of AD is still not completely understood. It was initially thought to be caused by genetic heritability (autosomal mutation leading to aggregation of β-amyloid and misfolded tau proteins) or head injury. However, hundreds of drug trials targeting the accumulation of sticky amyloid plaques and misfolded tau proteins in the brain have failed to yield any results. Although increasing evidence suggests that microbes and antimicrobial defense could play a critical role in causing AD (van den Pol 2009; Mawanda and Wallace 2013), the pathogenic microbes that contribute to AD onset and progression remain unknown.
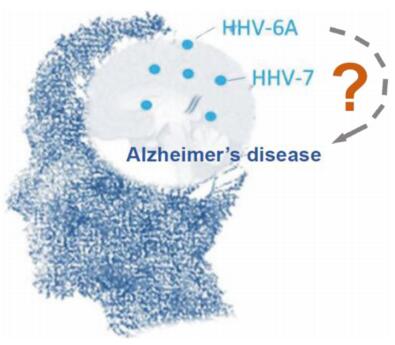
Human herpes viruses (HHVs) are common in the brains of the elderly (Kleinschmidt-DeMasters and Gilden 2001). Although they are usually dormant, they can become active in response to stress or if the immune system is compromised. The herpes simplex virus in particular is known to damage the central nervous system and the limbic system in the brain and it has been suggested that it may cause symptoms similar to AD (Bourgade et al. 2015). However, there is no strong evidence supporting the viral hypothesis and the link with AD has been suspected for a while. In a recent study, Readhead et al. (2018) developed a multiscale-network method, which they used to establish that two other common human herpesviruses, HHV-6A and HHV-7, could be key causal contributors to AD, although HSV co-infection was also observed in some cases. This study began by comparing the specific characteristics of two distinct AD-associated phenotypes, namely, individuals with preclinical AD, who were cognitively intact at the time of death, and cognitively intact persons without neuropathology, who served as the healthy controls. They next performed functional genomic analysis and found multiple lines of evidence of preclinical AD network alterations consistent with viral activity. These observations were further confirmed by viral and cellular RNA transcriptomic analysis of samples collected from patients with late-onset AD and neuropathologically and cognitively normal controls, as well as integrating -omic domain and diverse biomedical data from large patient cohorts including different disease stages and brain regions. This study provides compelling evidence that both HHV-6A and HHV-7 are linked to neuropathology and AD development. However, many questions regarding the characterization of these two viruses remain to be investigated (Fig. 1).
HTML
-
A single herpes virus can act in an unpredictable manner in infected individuals; infection in various regions of the brain can evoke different symptoms in only a small minority of infected individuals and infected individuals of varying ages may develop completely different syndromes. For instance, cytomegalovirus (a member of the β-herpesvirus subfamily) is considered to be the most common infectious agent capable of causing permanent dysfunction in the developing human brain; however, it poses little danger in mature individuals. Whether the other two members of this subfamily, HHV-6A and HHV-7, behave in a similar manner requires additional investigation.
According to Koch's postulates, which are the gold standard in establishing the microorganism causing an infectious disease, the organism must be found in every case of the disease and not found in those not afflicted with that particular disease. Obtaining the evidence required to confirm the HHV-6A and HHV-7 AD viral origin hypothesis is hindered by diversity. The link needs to be confirmed in an animal infection model using HHV-6A and HHV-7 separately and together, with observations of ADlike symptoms. In addition, because infections are less common in the brain than in other organs, the manner by which HHV-6A and HHV-7 penetrate the blood brain barrier and the mechanism by which HHV-6A and HHV-7 viral entry causes neurodegenerative disorders also need to be elucidated. Viral abundance analyses have revealed that in addition to HHV-6A and HHV-7, herpesviruses, such as human cytomegalovirus (HCMV), herpes simplex virus (HSV) 1, HSV2, HHV-6B, and Kaposi's sarcoma-associated herpesvirus (KSHV), are also present to some extent. Although Epstein-Barr virus (EBV) has not been observed in all groups in this study, it has been previously reported to infect neuron cells in vitro (Jha et al. 2015). This makes it more difficult to determine whether most herpesvirus infections are opportunistic pathogens that take hold in AD patients because of their compromised immune systems. An appropriate approach to determine which herpesviruses, if any, drive disease progression during the early phase of AD in patients carrying these viruses needs to be developed.
-
Viruses can cause neurological problems directly through many different mechanisms including viral lytic effects on brain cells and induced apoptosis. Given that murine roseolovirus (MRV), which is closely related to HHV-6A and HHV-7, has been shown to trigger apoptosis in developing thymocytes following primary infection (Komaroff et al. 2018), HHV-6A and HHV-7 infection could induce cell apoptosis. The activation of HHV-6A and HHV-7 lytic replication in infected neurons may also constitute a mechanism by which the virus causes brain damage. The immune response to viruses in the brain is complex and usually starts with the frontline innate neuronal and glial antiviral defenses; intriguingly, it has previously been reported that natural killer (NK) cells are activated in response to HHV-6A and HHV-7 infection through the STING-STAT6 pathway and that the infected NK cells produce high levels of cytokines IL-5 and IL-13 (Komaroff et al. 2018). Thus, indirect effects through the activation of the host immune response to HHV-6A/7-infected cells could also destroy brain tissue. As b-amyloid aggregation in AD has been accepted as part of an intra-central nervous system (CNS) innate immune response against microbe infection (Kumar et al. 2016), it is possible that the amyloid precursor protein (APP) pathway might be hijacked by HHV-6A/7 in the aging brain to cause damage.
In addition to microRNA miR-155, the authors also observed an increased abundance of the HSV1 encoded latency-associated transcript (LAT) and HHV-6A infection in multiple AD-brain regions across three independent clinical cohorts, which raised the possibility that HSV latent infection might be involved in HHV-6A-mediated AD progression (Readhead et al. 2018). One easy way to test this hypothesis would be to determine whether HSV reactivation from latency can block or delay HHV-6Amediated AD progression. That being the case, the next step would be to determine the underlying mechanism and which viral gene product (or LAT) is involved in this process. As AD is characterized by progressive neuronal cell loss mainly via apoptosis, it seems unlikely that LAT, a neuronal-cell-survival–enhancing factor, promotes AD progression. However, we have found that LAT can be trans-activated by host transcriptional factor ATF3 (Shu et al. 2015). Increased expression of ATF3 was found to be positively correlated with age-related amyloid-b deposition in an AD animal model (Zhu et al. 2014). Thus, it is still too early to rule out LAT as a viral candidate involved in AD progression; however, much remains to be done to substantiate this hypothesis.
-
It has been demonstrated that both HHV-6 and HHV-7 can integrate into subtelomeric regions of host chromosomes during latent infection and that they can be excised into an episomal form during lytic infection and replication (Tanaka-Taya et al. 2004; Prusty et al. 2017). The integrated process not only maintains the virus in silent (or reactivation) status, but also causes genetic mutations in the host; thus, integration could be a key mechanism by which these two viruses achieve latency and damage host cells. In addition, it would be useful to determine whether a single mutation within the viral genome could dramatically alter the ability of the viruses to subvert cellular antiviral defenses. In this study, the authors did not show whether the HHV-6A and HHV-7 genomes from late-onset AD tissues are highly present in a hot-spot mutation region. In addition, the virus might not exist in nature as a single genome, but rather as a population of closely related genomes in order to increase the success rate of infecting particular cell types (neuron or immune cells). For these reasons, it would be useful to determine a preferred cellular target in the brain for the virus or which virus clone, if any, might be responsible for a specific neurological problem.
The host antiviral defenses are complex and regulated by a variety of genes. Some alleles may protect the host from one specific type of viral infection, but increase susceptibility to others. In this study, the authors focused solely on which genes might modulate viral susceptibility; however, genetic differences among individuals undoubtedly contribute to the complexity of the CNS responses to viral invasion. They have revealed that seven modulators of the APP metabolism pathway are induced by HHV-6A and contribute to AD progression. However, only CLU, PICALM, and BIN1 were consistently observed in a previous report, which used genome-wide association studies in mega scale (Lambert et al. 2013). In addition, previous studies have shown that the CD46 receptor is the binding receptor for HHV-6A infection and that the absence of tolllike receptor 9 (TLR9) could contribute to HHV-6A-induced depression and anxiety in a mouse model (Komaroff et al. 2018). Further investigation is required to determine whether CD46 and TLR9 molecules are associated with HHV-6A infection in these cohorts, which would constitute an exciting discovery in the field.
In summary, this perspective study provides many possible future research directions examining both the mechanisms of herpesvirus-induced AD pathogenesis and potential approaches for treating AD by targeting herpesvirus infection. The related discoveries will undoubtedly contribute to the treatment of other progressive neurological diseases.
-
We thank all members in the lab for critical reading and discussion. This work was supported by the National Key Research and Development Program of China (2016YFC1200400). QC is a scholar of New Century Excellent Talents in University of China.
Acknowledgements
-
The authors declare that they have no conflict of interest.
-
This article does not contain any studies with human or animal subjects performed by any of the authors.













 DownLoad:
DownLoad: