-
Arden KE, Nissen MD, Sloots TP, MacKay IM. 2005. New human coronavirus, HCoV-NL63, associated with severe lower respiratory tract disease in Australia. J Med Virol, 75:455–462.
doi: 10.1002/(ISSN)1096-9071
-
Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, Alabdullatif ZN, Assad M, Almulhim A, Makhdoom H, Madani H, Alhakeem R, Al-Tawfiq JA, Cotten M, Watson SJ, Kellam P, Zumla AI, Memish ZA. KSA MERSCoV Investigation Team. 2013. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med, 369:407– 416.
doi: 10.1056/NEJMoa1306742
-
Bastien N, Anderson K, Hart L, Van Caeseele P, Brandt K, Milley D, Hatchette T, Weiss EC, Li Y. 2005. Human coronavirus NL63 infection in Canada. Clin Infect Dis, 191:503–506.
-
Cabeça TK, Granato C, Bellei N. 2013. Epidemiological and clinical features of human coronavirus infections among different subsets of patients. Influenza Other Respir Viruses, 7:1040–1047.
doi: 10.1111/irv.12101
-
Canducci F, Debiaggi M, Sampaolo M, Marinozzi MC, Berre S, Terulla C, Gargantini G, Cambieri P, Romero E, Clementi M. 2008. Two-year prospective study of single infections and coinfections by respiratory syncytial virus and viruses identified recently in infants with acute respiratory disease. J Med Virol, 80:716–723.
doi: 10.1002/(ISSN)1096-9071
-
Chiu SS, Chan KH, Chu KW, Kwan SW, Guan Y, Poon LL, Peiris JS. 2005. Human coronavirus NL63 infection and other coronavirus infections in children hospitalized with acute respiratory disease in Hong Kong, China. Clin Infect Dis, 40:1721– 1729.
doi: 10.1086/430301
-
Chung JY, Han TH, Kim SW, Kim CK, Hwang ES. 2007. Detection of viruses identified recently in children with acute wheezing. J Med Virol, 79:1238–1243.
doi: 10.1002/(ISSN)1096-9071
-
Dare RK, Fry AM, Chittaganpitch M, Sawanpanyalert P, Olsen SJ, Erdman DD. 2007. Human coronavirus infections in rural Thailand: a comprehensive study using real-time reverse-transcription polymerase chain reaction assays. J Infect Dis, 196:1321–1328.
doi: 10.1086/524219
-
Dijkman R, Jebbink MF, Gaunt E, Rossen JW, Templeton KE, Kuijpers TW, van der Hoek L. 2012. The dominance of human coronavirus OC43 and NL63 infections in infants. J Clin Virol, 53:135–139.
doi: 10.1016/j.jcv.2011.11.011
-
Ebihara T, Endo R, Ma X, Ishiguro N, Kikuta H. 2005. Detection of human coronavirus NL63 in young children with bronchiolitis. J Med Virol, 75:463–465.
doi: 10.1002/(ISSN)1096-9071
-
Esposito S, Bosis S, Niesters HG, Tremolati E, Begliatti E, Rognoni A, Tagliabue C, Principi N, Osterhaus AD. 2006. Impact of human coronavirus infections in otherwise healthy children who attended an emergency department. J Med Virol, 78:1609–1615.
doi: 10.1002/(ISSN)1096-9071
-
Fouchier RA, Hartwig NG, Bestebroer TM, Niemeyer B, de Jong JC, Simon JH, Osterhaus AD. 2004. A previously undescribed coronavirus associated with respiratory disease in humans. Proc Natl Acad Sci USA, 101:6212–6216.
doi: 10.1073/pnas.0400762101
-
Gaunt ER, Hardie A, Claas EC, Simmonds P, Templeton KE. 2010. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol, 48:2940–2947.
doi: 10.1128/JCM.00636-10
-
Hu Q, Lu R, Peng K, Duan X, Wang Y, Zhao Y, Wang W, Lou Y, Tan W. 2014. Prevalence and genetic diversity analysis of human coronavirus OC43 among adult patients with acute respiratory infections in Beijing, 2012. PLoS One, 9:e100781.
doi: 10.1371/journal.pone.0100781
-
Kaplan NM, Dove W, Abd-Eldayem SA, Abu-Zeid AF, Shamoon HE, Hart C. 2008. Molecular epidemiology and disease severity of respiratory syncytial virus in relation to other potential pathogens in children hospitalized with acute respiratory infection in Jordan. J Med Virol, 80:168–174.
doi: 10.1002/(ISSN)1096-9071
-
Koetz A, Nilsson P, Lindén M, van der Hoek L, Ripa T. 2006. Detection of human coronavirus NL63, human metapneumovirus and respiratory syncytial virus in children with respiratory tract infections in south-west Sweden. Clin Microbiol Infect, 12:1089–1096.
doi: 10.1111/j.1469-0691.2006.01506.x
-
Kuypers J, Martin ET, Heugel J, Wright N, Morrow R, Englund JA. 2007. Clinical disease in children associated with newly described coronavirus subtypes. Pediatrics, 119:e70–e76.
doi: 10.1542/peds.2006-1406
-
Lai MMC, Perlman S, Anderson LJ. 2007. Coronaviridae. In: Fields Virology, 5th ed. Knipe DM, Howley PM, Griffin DE, et al (Eds). Philadelphia: Lippincott Williams & Wilkins, pp. 1305.
-
Lau SK, Lee P, Tsang AK, Yip CC, Tse H, Lee RA, So LY, Lau YL, Chan KH, Woo PC, Yuen KY. 2011. Molecular epidemiology of human coronavirus OC43 reveals evolution of different genotypes over time and recent emergence of a novel genotype due to natural recombination. J Virol, 85:11325–11337.
doi: 10.1128/JVI.05512-11
-
Lau SK, Woo PC, Yip CC, Tse H, Tsoi HW, Cheng VC, Lee P, Tang BS, Cheung CH, Lee RA, So LY, Lau YL, Chan KH, Yuen KY. 2006. Coronavirus HKU1 and other coronavirus infections in Hong Kong. J Clin Microbiol, 44:2063–2071.
doi: 10.1128/JCM.02614-05
-
Liu WK, Liu Q, Chen de H, Liang HX, Chen XK, Chen MX, Qiu SY, Yang ZY, Zhou R. 2014. Epidemiology of acute respiratory infections in children in Guangzhou: a three-year study. PLoS One, 9:e96674.
doi: 10.1371/journal.pone.0096674
-
Mackay IM, Arden KE, Speicher DJ, O'Neil NT, McErlean PK, Greer RM, Nissen MD, Sloots TP. 2012. Co-circulation of four human coronaviruses (HCoVs) in Queensland children with acute respiratory tract illnesses in 2004. Viruses, 4:637–653.
doi: 10.3390/v4040637
-
McIntosh K, Kapikian AZ, Turner HC, Hartley JW, Parrott RH, Chanock RM. 1970. Seroepidemiologic studies of coronavirus infection in adults and children. Am J Epidemiol, 91:585–592.
doi: 10.1093/oxfordjournals.aje.a121171
-
Moes E, Vijgen L, Keyaerts E, Zlateva K, Li S, Maes P, Pyrc K, Berkhout B, van der Hoek L, Van Ranst M. 2005. A novel pancoronavirus RT-PCR assay: frequent detection of human coronavirus NL63 in children hospitalized with respiratory tract infections in Belgium. BMC Infect Dis, 5:6.
doi: 10.1186/1471-2334-5-6
-
Myint S, Johnston S, Sanderson G, Simpson H. 1994. Evaluation of nested polymerase chain methods for the detection of human coronaviruses 229E and OC43. Mol Cell Probes, 8:357–364.
doi: 10.1006/mcpr.1994.1052
-
Njouom R, Yekwa EL, Cappy P, Vabret A, Boisier P, Rousset D. 2012. Viral etiology of influenza-like illnesses in Cameroon, January-December 2009. J Infect Dis, 206:S29–S35.
doi: 10.1093/infdis/jis573
-
Oh MD, Choe PG, Oh HS, Park WB, Lee SM, Park J, Lee SK, Song JS, Kim NJ. 2015. Middle East Respiratory Syndrome Coronavirus Superspreading Event Involving 81 Persons, Korea 2015. J Korean Med Sci, 30:1701–1705.
doi: 10.3346/jkms.2015.30.11.1701
-
Patrick DM, Petric M, Skowronski DM, Guasparini R, Booth TF, Krajden M, McGeer P, Bastien N, Gustafson L, Dubord J, Macdonald D, David ST, Srour LF, Parker R, Andonov A, IsaacRenton J, Loewen N, McNabb G, McNabb A, Goh SH, Henwick S, Astell C, Guo JP, Drebot M, Tellier R, Plummer F, Brunham RC. 2006. An Outbreak of Human Coronavirus OC43 Infection and Serological Cross-reactivity with SARS Coronavirus. Can J Infect Dis Med Microbiol, 17:330–336.
-
Peiris JS, Lai S T, Poon L L, Guan Y, Yam LY, Lim W, Nicholls J, Yee WK, Yan WW, Cheung MT, Cheng VC, Chan KH, Tsang DN, Yung RW, Ng TK, Yuen KY, SARS study group. 2003. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet, 361:1319–1325.
doi: 10.1016/S0140-6736(03)13077-2
-
Pierangeli A, Gentile M, Di Marco P, Pagnotti P, Scagnolari C, Trombetti S, Lo Russo L, Tromba V, Moretti C, Midulla F, Antonelli G. 2007. Detection and typing by molecular techniques of respiratory viruses in children hospitalized for acute respiratory infection in Rome, Italy. J Med Virol, 79:463–468.
doi: 10.1002/(ISSN)1096-9071
-
Prill MM, Iwane MK, Edwards KM, Williams JV, Weinberg GA, Staat MA, Willby MJ, Talbot HK, Hall CB, Szilagyi PG, Griffin MR, Curns AT, Erdman DD; New Vaccine Surveillance Network. 2012. Human coronavirus in young children hospitalized for acute respiratory illness and asymptomatic controls. Pediatr Infect Dis J, 31:235–240.
doi: 10.1097/INF.0b013e31823e07fe
-
Regamey N, Kaiser L, Roiha HL, Deffernez C, Kuehni CE, Latzin P, Aebi C, Frey U. 2008. Viral etiology of acute respiratory infections with cough in infancy: a community-based birth cohort study. Pediatr Infect Dis J, 27:100–105.
-
Sloots TP, McErlean P, Speicher DJ, Arden KE, Nissen MD, Mackay IM. 2006. Evidence of human coronavirus HKU1 and human bocavirus in Australian children. J Clin Virol, 35:99–102.
doi: 10.1016/j.jcv.2005.09.008
-
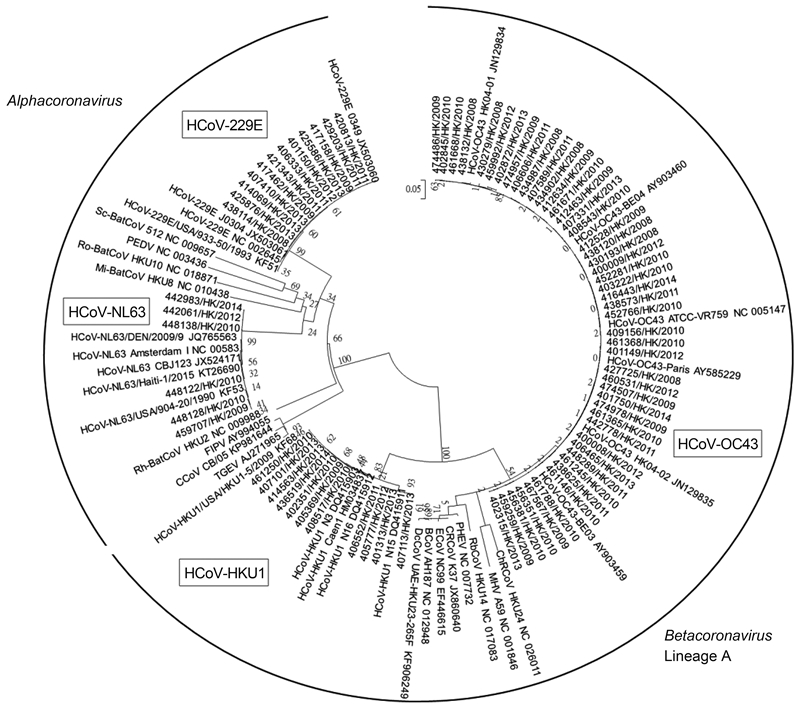
Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. 2011. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol, 28:2731–2739.
doi: 10.1093/molbev/msr121
-
Theamboonlers A, Samransamruajkit R, Thongme C, Amonsin A, Chongsrisawat V, Poovorawan Y. 2007. Human coronavirus infection among children with acute lower respiratory tract infection in Thailand. Intervirology, 50:71–77.
-
Vabret A, Dina J, Gouarin S, Petitjean J, Tripey V, Brouard J, Freymuth F. 2008. Human (nonsevere acute respiratory syndrome) coronavirus infections in hospitalised children in France. J Paediatr Child Health, 44:176–181.
doi: 10.1111/j.1440-1754.2007.01246.x
-
Vabret A, Mourez T, Gouarin S, Petitjean J, Freymuth F. 2003. An outbreak of coronavirus OC43 respiratory infection in Normandy, France. Clin Infect Dis, 36:985–989.
doi: 10.1086/cid.2003.36.issue-8
-
van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, Osterhaus AD. 2001. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med, 7:719–724.
doi: 10.1038/89098
-
van der Hoek L, Pyrc K, Berkhout B. 2006. Human coronavirus NL63, a new respiratory virus. FEMS Microbiol Rev, 30:760–773.
doi: 10.1111/j.1574-6976.2006.00032.x
-
van der Hoek L, Pyrc K, Jebbink MF, Vermeulen-Oost W, Berkhout RJ, Wolthers KC, Wertheim-van Dillen PM, Kaandorp J, Spaargaren J, Berkhout B. 2004. Identification of a new human coronavirus. Nat Med, 10:368–373.
doi: 10.1038/nm1024
-
Vijgen L, Keyaerts E, Moës E, Maes P, Duson G, Van Ranst M. 2005. Development of one-step, real-time, quantitative reverse transcriptase PCR assays for absolute quantitation of human coronaviruses OC43 and 229E. J Clin Microbiol, 43:5452–5456.
doi: 10.1128/JCM.43.11.5452-5456.2005
-
Woo PC, Chiu SS, Seto WH, Peiris M. 1997. Cost-effectiveness of rapid diagnosis of viral respiratory tract infections in pediatric patients. J Clin Microbiol, 35:1579–1581.
-
Woo PC, Lau SK, Chu CM, Chan KH, Tsoi HW, Huang Y, Wong BH, Poon RW, Cai JJ, Luk WK, Poon LL, Wong SS, Guan Y, Peiris JS, Yuen KY. 2005a. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol, 79:884–895.
doi: 10.1128/JVI.79.2.884-895.2005
-
Woo PC, Lau SK, Tsoi HW, Poon RW, Chu CM, Lee RA, Luk WK, Wong GK, Wong BH, Cheng VC, Tang BS, Wu A, Yung RW, Chen HL, Guan Y, Chan KH, Yuen KY. 2005b. Clinical and molecular epidemiological features of coronavirus HKU1-associated community-acquired pneumonia. J Infect Dis, 191:1898–1907.
doi: 10.1086/jid.2005.191.issue-11
-
Woo PC, Lau SK, Yip CC, Huang Y, Yuen KY. 2009. More and More Coronaviruses: Human Coronavirus HKU1. Viruses, 1:57–71.
doi: 10.3390/v1010057
-
Zumla A, Hui DS, Perlman S. 2015. Middle East respiratory syndrome. Lancet, 386:995–1007.
doi: 10.1016/S0140-6736(15)60454-8