-
Dear Editor,
The outbreak and rapid spread of the new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), have resulted in more than 120 million confirmed infections and 2 million deaths worldwide as of March 2021. The statistical data were from WHO COVID-19 Explorer (https://worldhealthorg.shinyapps.io/covid/). The virus is also responsible for billions of US dollars in economic losses and has attracted great concern about public health safety worldwide. Generally, patients who have been infected with SARS-CoV-2 have symptoms such as fever, dry cough, dyspnea, acute respiratory distress syndrome, and septic shock (Chen et al. 2020; Wu et al. 2020). SARS-CoV-2 has a strong capacity to survive and spread in respiratory droplets and aerosols, and it is essential to diagnose suspected cases accurately in the early stage of infection to avoid widespread infection. Here, we developed a nucleic acid molecular detection system targeting the N gene and ORF1ab gene for SARS-CoV-2 detection with CRISPR/Cas12a technology. This method has the advantages of high sensitivity and specificity due to the use of CRISPR/Cas12a technology, and it can be used for on-site testing with a portable testing instrument or immunochromatographic strips.
At present, the detection methods for SARS-CoV-2 are mainly focused on pathogen detection (Chu et al. 2020; El-Tholoth et al. 2020; Zhou et al. 2020), serological detection (Li et al. 2020; Zhang et al. 2020), and chest imaging detection (Xie et al. 2020). Every method has limitations; qRT-PCR, the gold standard for COVID-19 diagnosis (Chu et al. 2020) that is currently widespreadly used in laboratory and clinical detection, has a detection limit of 1 copy/μL (Supplementary Fig. S1A). However, due to its strict environmental requirements, qRT-PCR is not suitable for on-site detection, especially in public places such as airports, train stations, and seaports. Isothermal amplification technology (LAMP), such as real time LAMP (RT-LAMP), which greatly reduces detection cost and has relatively simple equipment requirements, is considered to be fit for on-site pathogen detection (Huang et al. 2020; Yan et al. 2020). The clustered regularly interspaced short palindromic repeats (CRISPR/Cas) based nucleic acid detection technology was developed to have the advantages of rapidity, simplicity, and low cost (Chen et al. 2018; Gootenberg et al. 2018). Combined detection systems have been applied to the detection of SARS-CoV-2, such as the CRISPR-based DETECTR method (Broughton et al. 2020) and the Cas13-based SHERLOCK system (Patchsung et al. 2020), which have their own advantages and disadvantages in detection conditions, time, and sensitivity (Table 1). RT-ERA reverses the template RNA into cDNA using the modified RNA reverse transcriptase. At the same time, the DNA recombinase combines with the primers to form a protein-DNA complex. The complex searches for and recognizes the homologous sequences in the cDNA and starts DNA synthesis (Xia and Chen 2020). The system amplifies specific genes exponentially within 20-30 min at constant temperature (37 ℃-42 ℃) with a sensitivity of 20 copies of SARS-CoV-2 N gene per reaction (Supplementary Fig. S1B). In this article, we combined RT-ERA with CRISPR/Cas12a to create a rapid and portable SARS-CoV-2 detection system. When the amplification system is added to the CRISPR/Cas12a system, Cas12a proteins cleave double-stranded DNA (dsDNA) with the specific crRNA guide, inducing robust, non-specific single-stranded DNA (ssDNA) trans-cleavage, but the specific cleavage mechanism is still unclear (Li et al. 2018). The ssDNA reporter fluoresces when the quenched fluorescent ssDNA is cleaved. We used a portable fluorescence constant temperature amplification instrument, namely the GS8 Isothermal Cycle, or immunochromatographic strips to collect and analyze fluorescence signals (Fig. 1A).
Detection systems Target Detection sensitivity (copies/µL) Assay reaction time (approximate) Assay components Bulky instrumentation required Reference OneStep RT-PCR assay N gene 1 90 min Denature (50 ℃, 15 min; 94 ℃, 15 min) amplification (94 ℃, 15 s; 55 ℃, 45 s; 45 cycles) Yes This study RT–LAMP ORF1ab gene 10 (ORF1ab) 60 min RT–LAMP (63 ℃ for 60 min) No Yan et al. (2020) S gene 100 (S) ORF1ab gene 0.08 30 min RT–LAMP (65 ℃ for 30 min) No Huang et al. (2020) S gene N gene RT–LAMP/Cas12 E gene 10 30–40 min RT–LAMP (62 ℃, 20–30 min) No Broughton et al. (2020) N gene Cas12 (37 ℃, 10 min) Cas13-based
SHERLOCK systemS gene 46.2 (S gene highest sensitivity) 60 min RT–RPA (42 ℃, 25 min) No Patchsung et al. (2020) ORF1ab gene Cas13 (37 ℃, 30–60 min) N gene RT-ERA N gene 10 80 min RT–ERA (39 ℃, 30 min) No This study Purification (56 ℃, 5 min) Agarose gel electrophoresis (45 min) Cas12a-based
RT-ERA systemN gene 0.25 (N) 40 min RT–ERA (39 ℃, 30 min) No This study ORF1ab gene 0.5 (ORF1ab) Cas12a (37 ℃, 10 min) Table 1. Comparison of detection methods for SARS-CoV-2
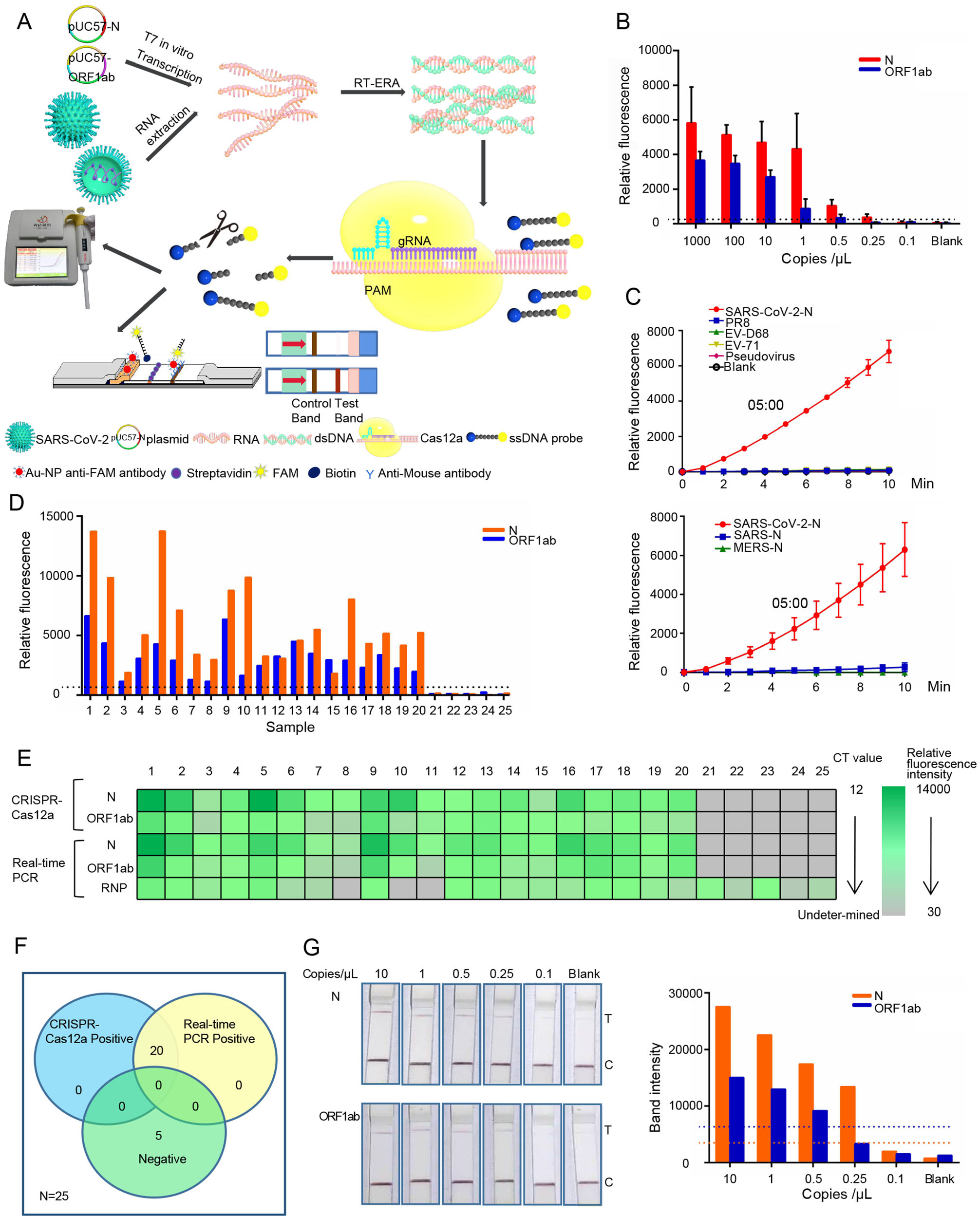
Figure 1. CRISPR/Cas12a technology combined with RT-ERA for SARS-CoV-2 detection. A Schematic diagram of Cas12a-mediated SARS-CoV-2 detection. The SARS-CoV-2 RNA transcribed in vitro or extracted from the virus was amplified by RT-ERA. After Cas12a was identified and combined with dsDNA under the guidance of crRNA, Cas12a randomly cleaved ssDNA FQ probe (F, fluorophore; Q, quencher), and then the fluorescence signal was collected by the GS8 Isothermal Cycler or immunochromatographic strips. B The histogram shows the sensitivity of CRISPR/Cas12a combined with RT-ERA for detection of N and ORF1ab genes at 10 min. Serially diluted synthetic SARS-CoV-2 RNA was used as a template. C The RNA of SARS-CoV-2 (100 copies/µL, N gene), influenza virus PR8 strain, enterovirus D68 (EV-D68), enterovirus 71 (EV71), and pseudovirus were amplified by RT-ERA and detected by the CRISPR/Cas12a system (upper panel). The N gene fragments of SARS and MERS were obtained by T7 transcription in vitro and detected as described above (lower panel). D The RNA was extracted from 25 clinical pharyngeal swabs and preamplified with RT-ERA for 30 min. The fluorescence signal was detected by the CRISPR/Cas12a system for 10 min. E The relative fluorescence value and Ct value of each clinical sample are displayed by a color scale diagram. F The Venn diagram shows the consistency between the CRISPR/Cas12a assay and the qRT-PCR assay. G The sensitivity of CRISPR/Cas12a combined with immunochromatographic strips for detection of N and ORF1ab genes (left panel). Serially diluted synthetic SARS-CoV-2 RNA was used as a template. The visualization of sample test band intensity was quantified by ImageJ and GraphPad (right panel)
Based on the sequence provided by the China CDC, we designed a specific crRNA for N and ORF1ab gene, which could be used to distinguish SARS-CoV-2 from other coronaviruses (SARS-CoV, MERS-CoV, HCoV-NL63, HCoV-229E, HCoV-OC43, HKU1, MHV, and IBV) (Supplementary Fig. S1C). And in order to improve the sensitivity of the detection system, we optimized the amplification and detection system to improve the amplification efficiency and shorten the detection time. In addition, we used a portable fluorescence isothermal amplification instrument, which is advantageous in its small size, easy operation, and automatic positive signal detection. Thus, the portable fluorescence isothermal amplification instrument is considered a good choice for on-site SARS-CoV-2 detection. This testing system can be used for on-site SARS-CoV-2 detection with a sensitivity of 7.5 copies of SARS-CoV-2 N gene and 15 copies of SARS-CoV-2 ORF1ab gene per 30-μL reaction (Fig. 1B), and the entire detection process takes only 40 min. The results of the cross-reactivity test with other tested viruses indicated that the SARS-CoV-2 CRISPR/Cas12a detection system had great specificity (Fig. 1C and Supplementary Fig. S1D). The results of CRISPR/Cas12a assay were in 100% agreement with qRT-PCR, meaning it correctly identified and differentiated all 20 positive samples and five negative samples, which were recruited from the Chinese Academy of Inspection and Quarantine (Beijing). (Fig. 1D-1F). There was no difference between the detection results of CRISPR/Cas12a and qRT-PCR detection for SARS-CoV-2. In order to simplify the field test equipment, we also combined the CRISPR/Cas12a system and immunochromatographic strips for detection (Fig. 1G). Although the band density was weak, there was a significant difference between the samples and the negative control group. It was demonstrated that the system has good sensitivity. We speculate that prolonging the incubation time may solve the problem of weak band density. In addition, the combination system also helped to ease the requirements of instruments for on-site detection. We showed that the combination of fluorescence detection and immunochromatographic strip detection was fast and had good sensitivity, and the detection of clinical samples could achieve 100% accuracy with qRT-PCR detection results (Fig. 1D-1F).
In summary, to promote the accurate diagnosis of suspected cases in the early stage of infection, we developed a rapid, highly sensitive, convenient SARS-CoV-2 detection method that utilizes RT-ERA amplification and the CRISPR/Cas12a system. This testing system can be used for on-site SARS-CoV-2 detection with a sensitivity of 7.5 copies of SARS-CoV-2 N gene and 15 copies of SARS-CoV-2 ORF1ab gene per 30-μL reaction in 40 min. Finally, we simplified the requirements for on-site detection instruments by using the CRISPR/Cas12a method combined with immunochromatographic strips, resulting in a powerful and effective tool for on-site detection of SARS-CoV-2 with high sensitivity and low cost.
HTML
-
We thank Y.-C. Zeng (Chinese Academy of Inspection and Quarantine) for technical advice. This work was supported by the National Key Research and Development Program of China (2017YFA0205102) and two independent innovation Foundations of Tianjin University (2020XY-0078 and 2020XY-0060).
-
All authors declare that they have no competing interests.
-
This study was approved by the local ethics committee of Tianjin University. Written informed consent was waived due to the rapid emergence of this infectious disease.















 DownLoad:
DownLoad: